Answering Common Questions on Dental Specializations
Dentistry encompasses a wide array of specialized fields, each focusing on distinct aspects of oral health and treatment. Understanding these various branches of dentistry can empower patients to navigate their dental care journey more effectively. Let's embark on a comprehensive exploration of each specialization to gain deeper insights:
1. General Dentistry: General dentists are like the family doctors of dentistry. General dentists serve as the primary providers of dental care for individuals of all ages. They offer a broad range of services aimed at maintaining oral health and preventing dental problems. General dentists also diagnose and treat common dental issues such as tooth decay, gum disease, and oral infections. They provide a wide range of dental services aimed at maintaining overall oral health. This includes routine examinations, cleanings, fillings, and preventive care such as fluoride treatments and sealants. General dentists are typically the first point of contact for patients seeking dental care and play a crucial role in promoting good oral hygiene habits
2. Periodontics: Periodontists specialize in the prevention, diagnosis, and treatment of diseases affecting the gums and supporting structures of the teeth. They are experts in managing conditions like gingivitis and periodontitis, performing procedures such as scaling and root planing, gum grafting, and periodontal surgery to restore gum health and preserve tooth stability. Also, They are experts in managing periodontal (gum) diseases, performing procedures such as scaling and root planing, gum grafting, and implant placement to restore gum health and prevent tooth loss
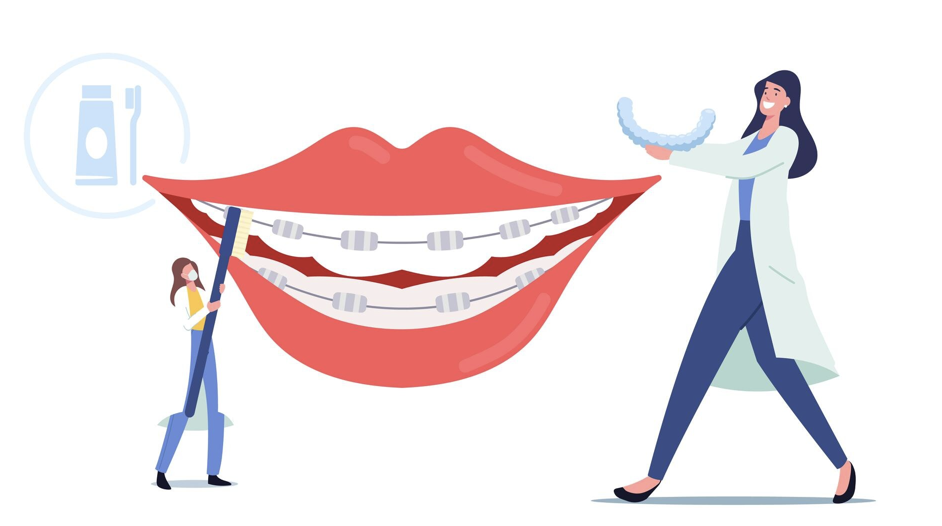
3. Orthodontics: Orthodontists focus on the diagnosis and treatment of malocclusions (misalignments of the teeth and jaws). They utilize various orthodontic appliances such as braces, clear aligners, and retainers to straighten teeth, correct bite issues, and improve overall dental function and aesthetics. Orthodontic treatment not only enhances the appearance of the smile but also contributes to long-term oral health.
4. Endodontics: Endodontists specialize in diagnosing and treating diseases of the dental pulp and root canal system. They perform root canal therapy to remove infected or damaged tissue from inside the tooth, effectively saving teeth that would otherwise require extraction. Endodontists also handle procedures like root canal retreatment and surgical endodontics to address complex cases.
5. Oral and Maxillofacial Surgery: Oral surgeons are skilled in performing surgical procedures involving the mouth, jaws, face, and neck. They address a wide range of conditions, including impacted wisdom teeth, jaw misalignments, facial trauma, oral pathology, and dental implant placement. Oral surgeons work closely with other dental specialists and medical professionals to provide comprehensive care to patients. Also, They handle a wide range of treatments, including tooth extractions (including wisdom teeth), dental implant placement, jaw surgery (orthognathic surgery), and treatment for oral diseases, infections, and injuries.
6. Pediatric Dentistry: Pediatric dentists specialize in providing dental care to infants, children, and adolescents. They focus on preventive care, early intervention, and education to promote lifelong oral health habits. Pediatric dentists create child-friendly environments and use techniques to ensure positive dental experiences for young patients, fostering a lifetime of good oral health.
7. Prosthodontics: Prosthodontists specialize in the restoration and replacement of missing or damaged teeth and oral structures. They design and fabricate dental prostheses such as crowns, bridges, dentures, and dental implants to restore function, aesthetics, and comfort for patients with compromised dentition. Prosthodontists employ advanced techniques and materials to create customized solutions tailored to individual patient needs.
8. Oral Pathology: Oral pathologists focus on the diagnosis and management of diseases affecting the oral and maxillofacial regions. They play a critical role in identifying oral cancers, oral infections, and other pathological conditions through comprehensive examination, biopsy, and laboratory testing. Oral pathologists collaborate with other dental specialists and healthcare providers to deliver timely and accurate diagnoses for optimal patient care.
Each of these dental specializations plays a vital role in preserving and enhancing oral health, addressing specific patient needs, and improving overall quality of life. By understanding the diverse fields of dentistry and the services they offer, patients can make informed decisions about their oral health care and embark on journeys toward healthier smiles and happier lives.
View Blog